
2021 MIPS Final Rule – Practical Information and Strategic Issues
Posted on December 7, 2020
Practical Information on 2021 MIPS, for those not participating in a MIPS APM
- Performance threshold: increases to 60 (up from 45), while the additional performance threshold stays at 85.
Why does this matter? This makes 2021 MIPS a little harder than 2020. The PT is the MIPS Final Score required to avoid a negative payment adjustment, and the APT is the MIPS Final Score to begin to earn additional positive payment adjustments for “exceptional performance.” CMS estimated that with the PT at 60, 24.4% of “engaged small practices” would receive a negative payment adjustment.
- Performance Category Weighting: Quality will be weighted at 40% (down from 45%), and Cost will increase to 20% (up from 15%).
The practice typically has greater control of its Quality score than its Cost score. That’s because Cost measures are Medicare PFS costs, notcosts to the practice. For most practices, shifting the balance from towards Cost will make 2021 MIPS a little harder.
- Complex Patient Bonus: (almost like a 5th MIPS performance category) will increase from 5% to 10%, but only for 2021.
Why is this important? These bonus points do not require additional reporting – they are calculated automatically by CMS based on claims – based on 2 measures: the mean HCC score of Medicare beneficiaries seen by the group or individual that year, and the percentage of dually eligible beneficiaries (Medicare and Medicaid). These bonus points boost your MIPS Final Score. This change will make 2021 MIPS a little easier.
- COVID-19 hardship exclusions: from any and all MIPS performance categories
will be available again for 2021, just like for 2020.This makes sense at one level, since we expect the pandemic to continue in 2021, but when you consider that the corresponding payment adjustments will be for the 2023 payment year, it makes less sense. See the BIG Takeaway, #9 below…
- Minor – Quality measures: have been updated as usual. 11 measures have
been removed, 113 have been modified, and 2 administrative claims measures
have been added (with Hospital Wide Readmission replacing the “classic” All-
Cause Hospital Admissions).Action item – review which CQMs you reported last year and cross compare with what has changed. This is normal – something you should do every MIPS performance year! CMS promises to publish the initial 2021 CQM spreadsheets prior to Jan. 1; if you want to review the CQM changes before CMS provides more convenient documentation, look at the Final Rule Appendix 1, ppg. 1,813 – 2,157, particularly “TABLE Group D” for CQMs with “Substantive Changes,” ppg. 2,014 – 2,157.
- Minor – Cost measures: have been updated to include tele-health services.
- Minor – Improvement Activities: have been updated as usual: 2 modified, 1 removed, and the COVID-19 clinical data reporting IA introduced mid-2020 will continue for 2021.
Chances are, IAs you’ve been reporting before have not been affected. IAs are the most misunderstood performance category in MIPS. If you want to figure out how to do these “right,” contact HiQ. The real reason to perform IAs is for the benefit of your practice and your patients, not for MIPS regulatory reasons.
- Minor – Promoting Interoperability measures: updated, as per the earlier 2021 MIPS Proposed Rule. This includes:
- Query PDMP bonus measure will double to 10 points (5 previously);
- A naming correction for an earlier CMS snafu: “Receiving / Incorporating Health Information” has been renamed to “Receiving / Reconciling Health Information”;
- An alternative, non-numeric (“yes/no”) HIE (Health Information Exchange) measure will be added, but with a very high performance threshold that electronic health information must be exchanged for all patient encounters, whether or not the patient had been referred. A generally excellent path for CMS to take – but they didn’t get the details right.
- Clarification that for 2021 CEHRT may be either classic 2015 Edition or 2015 Edition CURES Update, or a mix. CMS says it is “updating the CEHRT requirements” but really ONC had pre-empted this in an earlier ONCFinal Rule; ONC, not CMS, is redefining the term “2015 Edition Base EHR” according to an ONC schedule, thus implicitly changing the meaning of the CMS-defined term “CEHRT” – with CMS having nothing much to say about it.
- BIG take-away – Payment Adjustments: 2021 MIPS will be much like 2020 MIPS, and the final payment adjustment range is likely to be very small (0% to less than +2%), unless Congress and/or the new HHS Secretary and CMS Administrator take a significant new action to reinvigorate the MIPS program. The current MIPS performance category exclusion rules result in a neutral payment adjustment if excluding from 3 or 4 performance categories, which is to say not reporting at all or reporting only 1 performance category based on a valid exclusion such as related to COVID-19. So far, so good.
The current CMS administration, for whatever political, economic or population health management reason during the 2020 pandemic / election year, took unilateral action to say no MIPS eligible clinician would receive a negative MIPS payment adjustment for 2019 or 2020 performance! For 2019 (a pre-pandemic year, after all), the stated reason was that practices may have been disrupted from reporting for 2019 during Q1 of 2020 during the initial pandemic wave – no exclusion filing was required; for 2020, the explanation was that the pandemic may have prevented practices from performing normally, with a performance category specific hardship exclusion filing required. The justification for waiving negative payment adjustments altogether was to encourage MIPS reporting without an unfair risk of a negative payment adjustment.
Since MACRA requires MIPS to be budget-neutral except for a $500M/yr budget for “exceptional performance” during the first 6 years, these unilateral CMS decisions to blanketly waive negative payment adjustments resulted in the highest positive payment adjustment for 2019 performance being limited to only +1.79%, rather than the +4.69% which CMS had previously estimated; similarly, the maximum payment adjustment for 2020 performance (which will only be announced Q3/2021) can also be expected to be below +2%, rather than the +6.25% which CMS had previously estimated. This has been, and will continue to be, a big disappointment to practices who have been working hard to perform at truly exceptional levels of performance and were counting on higher, promised and much-needed financial rewards.
Let’s digress and talk about what perhaps should have happened. Admittedly, a negative financial impact of MIPS on practices struggling during the pandemic was something which made sense for the government to avoid – especially negative payment adjustments for the 2020 payment year, based on 2018 performance, for which unfortunately no relief was provided. Congress perhaps should have passed emergency legislation to waive negative MIPS payment adjustments for the 2020 and 2021 payment years due to the pandemic, while still maintaining high positive MIPS payment adjustments for practices who had rightfully earned them; for 2019, Congress perhaps should have required CMS to calculate the 2021 positive payment adjustments based on the estimating hypothetical negative payment adjustments for low performers, even though those negative payment adjustments would be waived. That way, no practices would have been negatively affected by MIPS during the pandemic, and top performers would have received much-needed approximately +4.99% payment adjustments in 2021 and approximately +6.25% in 2022. That would have made sense! C’est la vie….
If CMS were to use the same “logic” for unilateral action to waive all negative payment adjustments for 2021 performance, the maximum positive MIPS payment adjustment would again end up below +2%, in this case for the 2023 payment year. In the 2021 Final Rule, the current CMS administration still talks about a +7.36% maximum positive payment adjustment for 2021 performance, but that is entirely misleading and would depend on Congress acting and/or HHS and CMS changing course.
In a sense, CMS has short-circuited the original Congressional intent for MIPS by shifting the intended bell-shaped curve of significant negative vs. positive payment adjustments, based on performance and with the average provider receiving a neutral payment adjustment, to a public handout of exclusively neutral or very small positive payment adjustments, with the average provider receiving a petty portion. MIPS is a lot of heavy-weight CEHRT, registry, submission and payment adjustment machinery for such a very small financial impact per provider! Instead of encouraging competition and high performance, the HHS and CMS administration has turned MIPS payment adjustments into a provider welfare system not significantly benefiting anyone!
Action item: providers can act by contacting their Congressman / Congresswoman and asking their professional societies to lobby Congress to reinvigorate the MIPS program, so that that high performers receive high positive payment adjustments! Demand that the promised +7.36% be awarded for a perfect 2021 MIPS Final Score!
Practical Information on 2021 MIPS, for MIPS APM participants
APP (APM Performance Pathway) is being introduced for 2021, “complementary to MVPs” even though MVPs are not being introduced in 2021, to change how MIPS APM performance is reported and scored. APP may be reported by the individual participant, by the participant’s group, or by the MIPS APM Entity (e.g. the ACO). Quality measures must be reported from a small fixed set of measures (see table below); the CMS Web Interface will continue to be allowed for 2021 only. The Cost performance category is waived and the Improvement Activities performance category will be fully credited for APM participation for 2021. Promoting Interoperability must be reported at the individual and/or group level and is aggregated for the APM Entity by CMS.
The APP quality measures are shown in the table below (Table #40 in the Final
Rule):
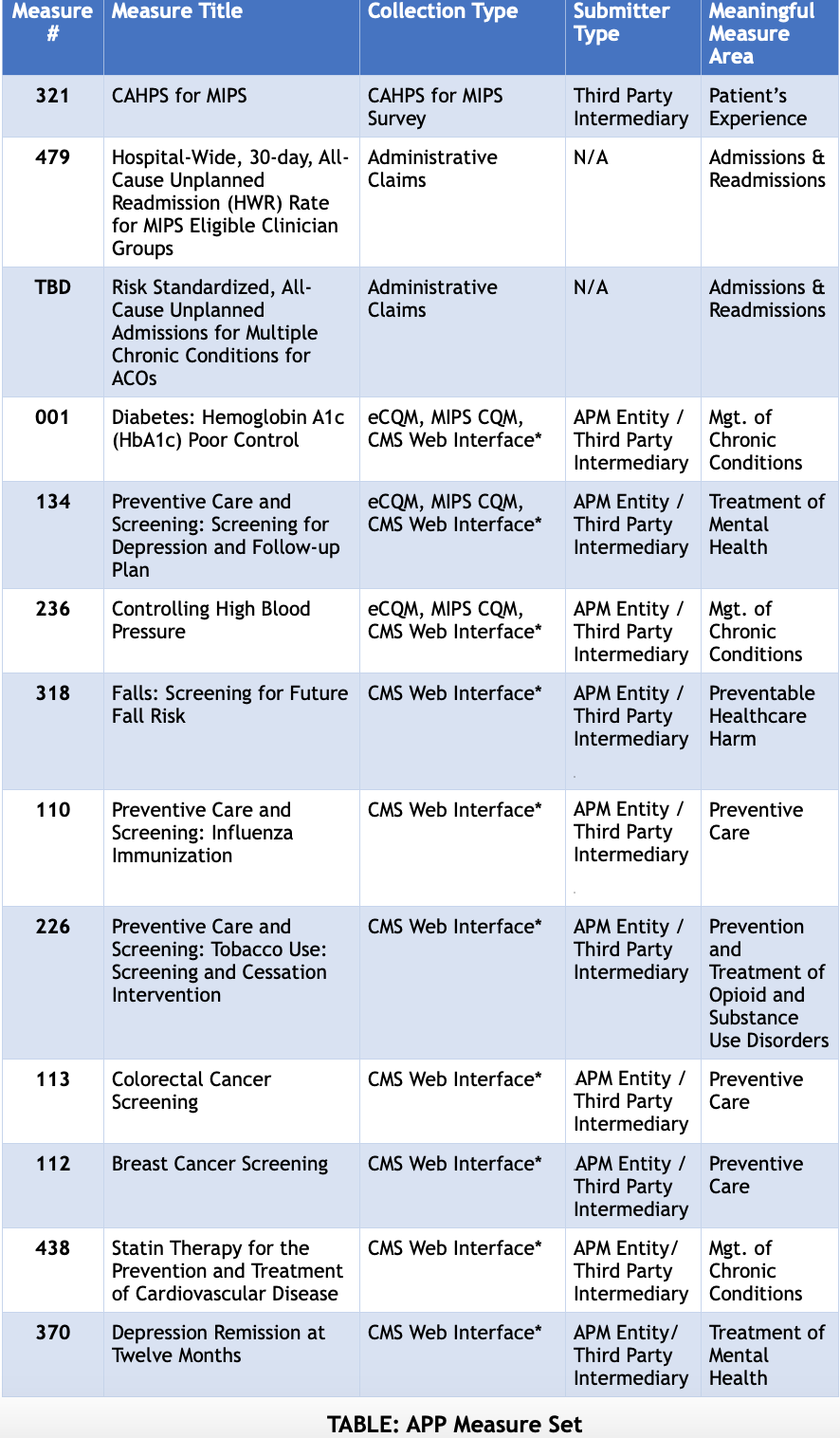
If not using the CMS Web Interface 7 out of 10 of its measures do not need to be reported.
As already pointed out in a previous HiQ blog article on the Proposed Rule earlier this year, the problem with this APP mechanism is that, unlike the concept for MVPs, it is designed only for primary care and does not properly support specialty-specific APMs – presumably the best the CMS team could come up with. Expect further rework of this concept in future rule-making.
Strategic Issues for 2022 MIPS and MVPs
- Retroactive Calculation of Performance Thresholds. Starting in 2022, the key MIPS Final Score thresholds (PT and APT) will no longer be pre-determined by CMS, but will be calculated retro-actively based on the 2022 performance year’s mean or median MIPS Final Score, as required by MACRA.
CMS had previously estimated that the 2022 PT might be 74.01, which would imply an APT of 80.51, but the real values are almost guaranteed to be different. More recently, CMS estimated that the 2019 MIPS mean score was 79.8 and the median 85.27. Count on CMS picking the mean to make the first “non-transition year” easier. HiQ prediction: the PT will be approximately 80, and the APT will be approximately 85.
This will make MIPS significantly harder, particularly for small practices who have been scoring lower than large practices!
- Balancing of Quality and Cost– they will both be weighted at 30% (except for MIPS APMs_, as required by MACRA.
As explained for 2021 Quality vs. Cost weighting, this will make 2022 harder.
- MVPs (MIPS Value Pathways) may be introduced, although they would be optional at first. MVPs are such a major restructuring of MIPS that CMS introduced the term “traditional MIPS” for how things are now. CMS also used the terms “Meaningful Measures” and “Meaningful MVPs” repeatedly in the Final Rule, which should rightfully cause rightful apprehension and a feeling of déjà vu for those with a bitter aftertaste from “Meaningful Use.” As good a place as any to start worrying about MVPs is with the “Guiding Principles for MVPs” that CMS (not Congress) has defined:
- “MVPs should consist of limited, connected complementary sets of measures and activities that are meaningful to clinicians, which will reduce clinician burden, align scoring, and lead to sufficient comparative data.”
- Careful with the terms “limited” and “align scoring” and “comparative data” –CMS wants to eliminate MIPS quality measure selection flexibility and force all providers of the same specialty to report the same measures – even if CMS doesn’t really understand the specialties or sub-specialties.
- CMS loyalists might argue that CMS has intended MVPs not only per specialty, but possibly per condition or “episode of care” (they probably meant “type of episode of care”). However, the more CMS facilitates introducing a plethora of MVPs, the more it undercuts its own goals to “align scoring and lead to sufficient comparative data.” You can’t have your cake and eat it too.
- Careful with the “activities” – CMS is talking about Improvement Activities and wants all providers within the same specialty to perform the same ones – even though experience with quality improvement and quality management systems teaches us that quality initiatives are more effective when initiated “bottom up” rather than “top-down” as in centralized planning! For example, CMS had suggested that ophthalmologists may be required to perform the “Comprehensive Eye Exams” IA – which superficially sounds perfect, but on closer reading means they may need to participate in AAO’s “EyeCare America” program to provide free exams to the underserved – a noble goal but not necessarily appropriate to be a federal government mandate! Truth is most of the IAs are not specialty specific – which is a good thing!
- Watch that “meaningful” part! It already “means” something to us – as in “Meaningful Use” and not necessarily a good thing!
- “MVPs should include measures and activities that would result in providing comparative performance data that is valuable to patients and caregivers in evaluating clinician performance and making choices about their care; MVPs will enhance this comparative performance data as they allow subgroup reporting that comprehensively reflects the services provided by multispecialty groups.”
- Careful with that “patients and caregivers … evaluating clinician performance” phrasing – especially in the age of prescription drug ads on television! Patient-Centered Care: yes! Patient-Reported Measures: yes! Patient evaluation of clinician performance: no!
- “Subgroup reporting” is one of the few really good ideas in MVPs – it means reporting in-between the TIN and the TIN-NPI level, such as for all of the providers in a group in the same specialty, or subspecialty. Remember that MIPS Final Scores are always awarded at the individual level (for the TIN-NPI pair), no matter if the score came from individual, group, virtual group, or MIPS APM Entity reporting. This is one of the things Congress forgot to micro-specify in MACRA. Sadly, CMS is not currently intending to allow this concept of “subgroup reporting” for “traditional MIPS.”
- “MVPs should include measures selected using the Meaningful Measures approach and, wherever possible, the patient voice must be included, to encourage performance improvements in high priority areas.”
- There they go again! What does “Meaningful Measures” actually mean? In the Final Rule, the closest CMS comes to explaining it is:
“We intend to work with stakeholders to develop MVPs that include meaningful measures…”
In other words, CMS doesn’t really know what meaningful measures are, but will work with stakeholders (as in professionals and their societies) to develop them. But wait! Haven’t those professional societies already developed measures, and aren’t they already MIPS CQMs or QCDR measures, and isn’t that already an ongoing effort? So let’s see what the CMS website has to say about it:
“’Meaningful Measures’ framework is the Centers for Medicare and Medicaid Services’ new initiative which identifies the highest priorities for quality measurement and improvement.
It involves only assessing those core issues that are the most critical to providing high-quality care and improving individual outcomes. The Meaningful Measure Areas serve as the connectors between CMS strategic goals and individual measures/initiatives that demonstrate how high quality outcomes for our beneficiaries are being achieved. They are concrete quality topics, which reflect core issues that are most vital to high quality care and better patient outcomes.Examples of Meaningful Measure Areas include Healthcare Associated Infections and Prevention and Treatment of Opioid and Substance Use Disorders. Each of these Meaningful Measure Areas helps to make the connection to specific CMS strategic goals such as ‘Empower patients and doctors to make decision about their health care’ and ‘Support innovative approaches to improve quality, safety, accessibility, and affordability’ through depicting core issues that are broader than a given individual measure.”
Okay… that sounds very general and vague. But wait, there’s a diagram below the explanation! Maybe that will explain what “Meaningful Measures” are!
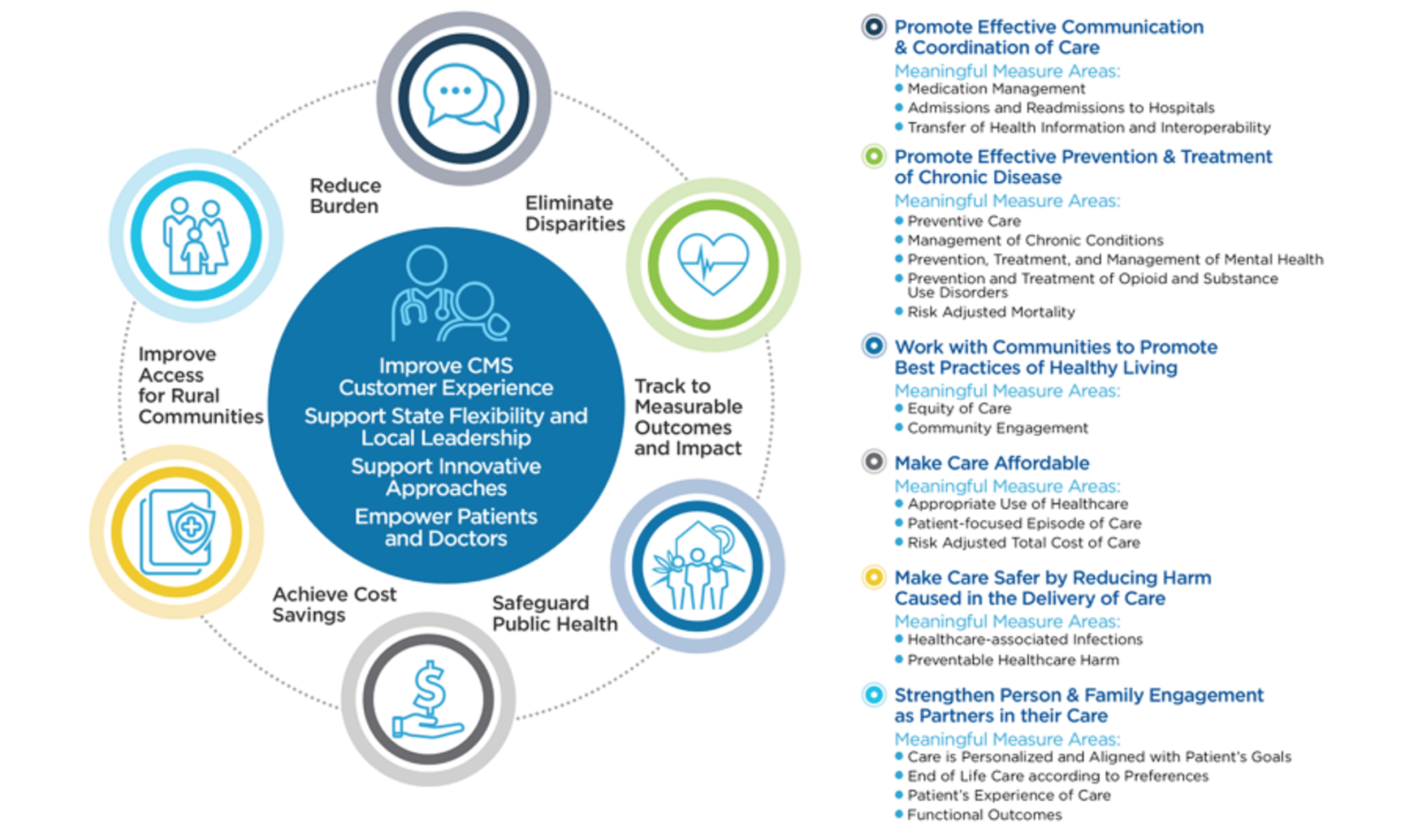
Okay… that’s starting to look scary, a little like a WHO initiative but definitely like a “Grand Framework” project! As an aside – Grand Framework projects almost always fail…. Let’s go backwards in time and see how this “Meaningful Measures” thing actually originated. Apparently, it all started in 2017 – coincidentally the first year of MIPS! Here’s how it read back then:
“Launched in 2017, CMS’s new comprehensive ‘Meaningful Measures’ initiative identifies high priority areas for quality measurement and improvement to improve outcomes for patients, their families, and providers while also reducing burden on clinicians and providers.”
“The Meaningful Measures initiative draws on prior measure work performed by the Health Care Payment Learning and Action Network, National Quality Forum, and National Academies of Medicine. It includes perspectives from patient representatives and additional experts such as the Core Quality Measures Collaborative, and many other external stakeholders.”
“Principles for Identifying Meaningful Measures
Meaningful Measures will move payment toward value by focusing everyone’s efforts on the same quality areas and advancing specificity by identifying measures that:
- Are patient-centered and meaningful to patients, clinicians, and providers
- Address high-impact measure areas that safeguard public health
- Are outcome-based where possible
- Minimize level of burden for providers
- Create significant opportunity for improvement
- Address measure needs for population based payment through alternative payment models
- Align across programs”
Okay… that still sounds like a Grand Framework project, but it makes a little more sense, maybe because it was still closer to the input provided by NQF and other non-government organizations.
- There they go again! What does “Meaningful Measures” actually mean? In the Final Rule, the closest CMS comes to explaining it is:
- “MVPs should reduce barriers to APM participation by including measures that are part of APMs where feasible, and by linking cost and quality measurement.”
- Wasn’t reducing barriers to APM participation built into QPP – by having MIPS and advanced APMs tracks within QPP, and a MIPS APMs sub-track within MIPS?
- Isn’t the real barrier to APM participation that there are insufficient specialty APMs? And wouldn’t development of suitable specialty APMs be a higher priority initiative than MVPs?Wouldn’t harmonizing MIPS measures with current APMs measures (such as APP, see above) entirely “dumb down” the measurement process for specialists?
- Wasn’t the basic idea behind MIPS to link cost and quality measurement, resulting in a hybrid MIPS Final Score?
- “MVPs should support the transition to digital quality measures.”
- The Final Rule tells us to read the Proposed Rule to see what this means:
“Digital Quality Measures (dQMs) originate from sources of health information that are captured and can be transmitted electronically and via interoperable systems. Examples of digital sources include electronic health records (EHR), health information exchanges (HIEs), clinical registries, case management systems, electronic administrative claims systems, electronically submitted assessment data, and wearable devices. Electronic clinical quality measures or eCQMs (data derived from electronic medical records) are a subset of dQMs.”
“Wearable devices”? Does CMS intend to give everyone smart watches and collect all the data, to make sure everyone is doing enough walking steps each day, otherwise they ding the responsible physician for bad Preventive Medicine?
- Another clue about what this means is the CMS master diagram for MVPs, which includes the following easily-overlooked part at the bottom:
 To interpret this diagram, the “Clinician / Group reported data” which currently predominates will be matched by “CMS provided data” – dQMs means that CMS will want to ramp up its ability to capture your performance in ways other than you reporting certified measures from your own electronic healthcare records, even if your professional society is reporting them via QCDR! CAHPS patient surveys and other patient-reported measures make sense, but a comprehensive big-brother espionage program does not, especially if you don’t know where the data is coming from! They want to ramp them up other sources of information to nearly 50% of the info they have on you! Is that a good thing?
To interpret this diagram, the “Clinician / Group reported data” which currently predominates will be matched by “CMS provided data” – dQMs means that CMS will want to ramp up its ability to capture your performance in ways other than you reporting certified measures from your own electronic healthcare records, even if your professional society is reporting them via QCDR! CAHPS patient surveys and other patient-reported measures make sense, but a comprehensive big-brother espionage program does not, especially if you don’t know where the data is coming from! They want to ramp them up other sources of information to nearly 50% of the info they have on you! Is that a good thing?
Action item: providers wary of MVPs, Meaningful Measures and dQMs can act by contacting their Congressman / Congresswoman and asking their professional societies to lobby Congress to:
- The Final Rule tells us to read the Proposed Rule to see what this means:
- re-evaluate the MVPs framework;
- limit the Meaningful Measures and dQMs concepts since they appear to be a boondoggle and undermine clinical data registries and detailed, objective evidence;
- allow subgroup reporting for “traditional MIPS”; and
- charge CMS to collaborate with specialty societies to develop suitable specialty APMs.
- “MVPs should consist of limited, connected complementary sets of measures and activities that are meaningful to clinicians, which will reduce clinician burden, align scoring, and lead to sufficient comparative data.”
Remember that CMS, as a government agency, is supposed to serve you – not the other way around!
Recent Posts
- 2021 MIPS Final Rule – Practical Information and Strategic Issues December 7, 2020
- HiQ Adds Platinum Tier to MIPS EssentialsTM Service September 21, 2020
- 2021 MIPS Proposed Rule August 7, 2020
- Waiting for MVPs June 25, 2020
- Webinar – Interoperability and the Practice – June 24, July 8, & Aug 5,2020 May 11, 2020
