2021 MIPS Proposed Rule
Posted on August 7, 2020
CMS Proposed Rule for 2021 MIPS: One Big Nothing Burger
We shouldn’t be surprised that CMS decided to punt by postponing its long-heralded introduction of “MIPS Value Pathways” (MVPs):
“We intended to begin transitioning to MVPs in the 2021 MIPS performance year; however, due to the 2019 Novel Coronavirus (COVID-19) pandemic public health emergency and resultant need for clinician focus on the response, our timeline has changed accordingly such that the proposal for initial MVPs will be delayed until at least the 2022 performance year.”
MVPs was lauded as a restructuring of MIPS to “simplify” the program, but with the hidden agenda of making scoring harder and reducing the median score from its 2018 “topped out” value of 99.63 out of 100. MVPs was supposed to ensure that all MIPS eligible clinicians within a given medical specialty would be subject to the same measures for a fair “apples-to-apples” comparison, both for MIPS scoring and for Physician Compare. CMS had previously proposed to introduce MVPs in 2021 but making them optional for at least the first year and thus without any “teeth”. However, it seems likely that the pandemic is just an excuse and that CMS was simply not ready for MVPs at this time.
So what is in the 2021 MIPS Proposed Rule?
CMS is proposing a hodge-podge of changes for the 2021 MIPS performance year:
- Removing the CMS Web Interface as a quality measure “collection type” for 2021. This change will not affect small practices.
- Lowering the previously announced 2021 Performance Threshold from 60 to 50. This represents the MIPS Final Score needed to avoid a negative payment adjustment. The lower rate of increase is explained as a pandemic accommodation, but will result in lower maximum positive payment adjustments for the 2023 payment year.
- Lowering the previously announced 2021 weighting balance between Quality and Cost from 35% / 25% to 40% / 20%. Despite this hesitation on the part of CMS for 2021, CMS will be required by law to set this balance at 30% / 30% starting with the 2022 MIPS performance year.
- The Complex Patients Bonus score will be increased from 5 to 10 points towards the MIPS Final Score, for one year only, as a pandemic accommodation. This score is based on two measures of the provider’s Medicare patients as computed automatically by CMS: the percentage of Medicare patients who are “dually eligible” for Medicaid as well, and the average patient HCC (Hierarchical Condition Code) score. This bonus score may help MIPS eligible clinicians get closer to a perfect MIPS Final Score.
- Increasing the PDMP bonus measure for Interoperability from 5 to 10 points. This is an optional “yes/no” measure attesting to use of electronic queries of the applicable state Prescription Drug Monitoring Program and may help MIPS eligible clinicians get closer to a perfect Promoting Interoperability score.
- Adding a new, optional “HIE bi-directional exchange” measure for Interoperability, as an alternative to the two “Direct messaging” measures “Sending Health Information” and “Receiving / Reconciling Health Information”. Particularly interesting is that this is a non-numeric measure only requiring “yes/no” attestation, also perhaps making a perfect Interoperability score feasible – however see further analysis below for its risks.
- APP (APM Performance Pathway) is being introduced for 2021 as “a complementary Pathway to the MVPs” (even though MVPs are not being introduced). This applies to any MIPS APM participant, and is somewhat of a terminology game, perhaps for CMS to be able to say that they did introduce some type of “pathway”. APP may be reported by the individual participant, by the participant’s group, or by the MIPS APM Entity (e.g. the ACO). Quality measures must be reported from a fixed set of 6 measures (see table and further analysis below). As before for MIPS APM scoring, the Cost performance category is waived and theImprovement Activities performance category will be fully credited for APM participation for 2021 (essentially waived).
- It goes without saying that there are annual changes to Quality and Cost measures as well as Improvement Activities.
The high risk burden of the new HIE Bi-Directional Exchange measure
The new Promoting Interoperability measure for HIE Bi-Directional Exchange may seem a tempting alternative to the “standard” measures of “Sending Health Information” and “Receiving / Reconciling Health Information”, however it carries a high risk burden in case audited:
- The data set for each patient must be supported by CEHRT and must include the current CCDS (Common Clinical Data Set) or in the near future the expanded USCDI (United States Core Data for Interoperability);
- Standard workflow must be to query the HIE and reconcile the data set for all new and existing patients prior to or during an office visit;
- Standard workflow must be to post updated health information to the HIE for all patients following the office visit;
- Limited HIEs such as within a single healthcare organization or only involving healthcare providers using the same CEHRT are not eligible;
- CMS emphasizes that the greater flexibility of this measure is tied to the significantly higher threshold of performance expected (equivalent to a perfect score on the “standard” care coordination measures) and subject to audits.
What’s wrong with the new APM Performance Pathway?
Very simply, the APP quality measure set is fixed and is only sensible for primary care, as per the following table from the Proposed Rule:
TABLE 41: APM Performance Pathway Quality Measure Set
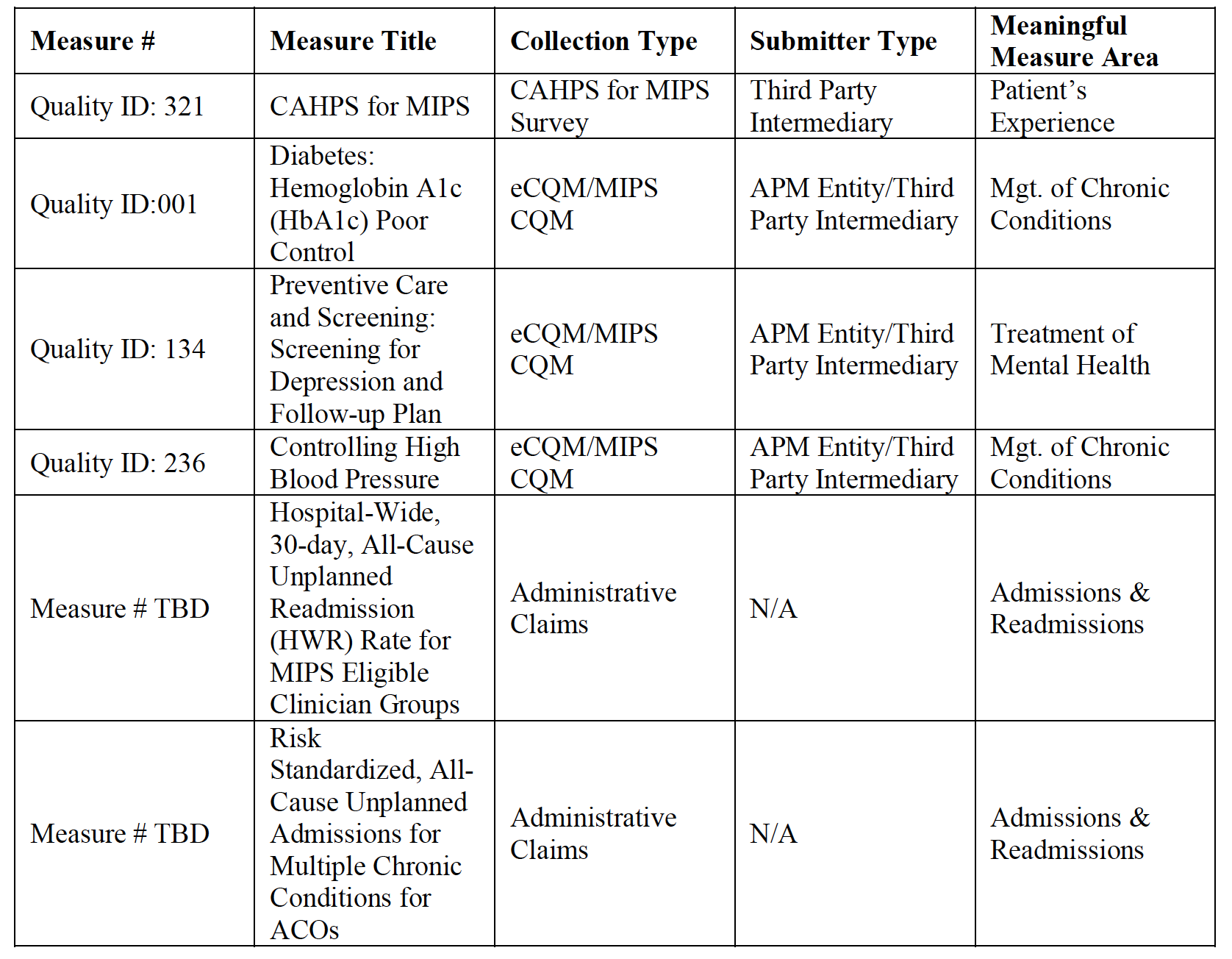
This fixed set of primary care measures for APP is entirely at odds with the basic concept of MVPs, to select measures according to medical specialty. While the above may make sense for primary care APMs, it makes no sense for medical specialty APMs, and is somewhat of a faux-pas in the Proposed Rule which may possibly be corrected in the Final Rule. Basically, a correction in the Final Rule might assign alternate APP measure sets for existing specialty APMs, selecting 6 appropriate measures from the applicable existing Quality specialty measure set.
Will we see MVPs in 2022?
Maybe. Maybe not.
The 2022 MIPS performance year will be dominated by a different, major and unavoidable set of rule changes, as required by law:
- The MIPS Performance Threshold (the MIPS Final Score required to avoid a negative payment adjustment) will no longer be predetermined. Rather, CMS will be required to use the nationwide median (or mean) MIPS Final Score as the Performance Threshold for scoring from that year on. The 2022 Performance Threshold will only be known after the performance year has completed and will be much higher than the 50 points proposed by CMS for 2021. That will make 2022 MIPS much more difficult, because by definition approximately half of providers nationwide will “fail” in the sense of earning a negative payment adjustment.
- Similarly, the “Additional Performance Threshold” (the MIPS Final Score required to begin to earn additional payment adjustments for “exceptional performance”) will also not be predetermined. This will be calculated as the first quartile between the Performance Threshold and a perfect score of 100.
- Quality and Cost are required to be weighted equally: 30% of the MIPS Final Score each.
For the 2022 MIPS performance year, program participants, at least those paying attention, will want to focus on improving their measured MIPS performance so as to stay above the nationwide average and thus avoid negative payment adjustments. This will not be a “good” year for CMS to begin completely restructuring the program. Thus, we may not see MVPs until 2023, and if MVPs will be optional the first few years, we may not see MVPs in full effect until perhaps 2025.
So, Where’s the Beef?
The gist of the Proposed Rule is to make the 2021 MIPS performance year easier than previously planned – via a deferral of MVPs, a lower Performance Threshold, lower weight for Cost performance, higher Complex Patients and PDMP bonus points and the alternative, non-numeric HIE measure for care coordination. The net effect for 2021 will be to:
- Keep the MIPS median score high;
- Prevent a significant number of MIPS eligible clinicians from receiving negative payment adjustments;
- Lower the maximum possible positive MIPS payment adjustment (since the payment adjustments must be budget neutral);
- Decrease healthcare provider focus on MIPS (other than for a minimum level of participation) due to low financial impact;
- Undermine the bi-partisan goals for value-based care Congress had set with MACRA in 2015.
CMS will have missed the opportunity to use the first 5 MIPS performance years (2017 through 2021 – the “transition years”) to achieve a very basic, measurable goal of ensuring that the MIPS Final Score is not a “topped out”.
If everyone gets a gold star, the gold stars are meaningless. In terms of financial impact, if the MIPS median score is topped out, the maximum possible positive payment adjustment will be very low. The net result will be that MIPS is transformed back into a Meaningful Use / PQRS style “penalty program” – the main incentive will be to avoid the penalty by achieving at least close to the nationwide average score.
We should not be surprised if Congress acts with follow-up legislation to MACRA to force CMS to restructure the program so as to have the composite Final Score a meaningful measure of performance for quality of care, cost of care, clinical practice improvement activities and use of CEHRT for interoperability.
Recent Posts
- 2021 MIPS Final Rule – Practical Information and Strategic Issues December 7, 2020
- HiQ Adds Platinum Tier to MIPS EssentialsTM Service September 21, 2020
- 2021 MIPS Proposed Rule August 7, 2020
- Waiting for MVPs June 25, 2020
- Webinar – Interoperability and the Practice – June 24, July 8, & Aug 5,2020 May 11, 2020
