
Waiting for MVPs
Posted on June 25, 2020
What do we know about MVPs so far?
We should soon see the CMS Proposed Rule for the 2021 MIPS performance year but will then need to wait again until November for the corresponding Final Rule. The main topic of interest for MIPS will be “MVPs” (MIPS Value Pathways), which CMS has promised to begin phasing in over a period of years starting with the 2021 MIPS performance year. CMS tells us MVPs are intended to restructure and “simplify” the MIPS program.
In the 2019 calendar year rule-making cycle (targeting the 2020 MIPS performance year), CMS had already given us early warning of MVPs but only provided broad concepts, posing more questions for public comment than offering firm specifics. A number of industry pundits then immediately rushed to summarize the 2019 CMS MVPs concepts, but mostly in a non-critical manner without analyzing the subject in greater depth and without much value-added.
CMS has since created a web page for MVPs at:
https://qpp.cms.gov/mips/mips-value-pathways
CMS conducted and recorded several public webinars on MVPs, the most recent of which was held in March, 2020; the interested reader is encouraged to take the time to view this recording:
https://youtu.be/nNk9RLDW9zE
CMS has tried to follow the adage that “a picture is worth a thousand words” and provided us with the following diagram to explain MVPs:
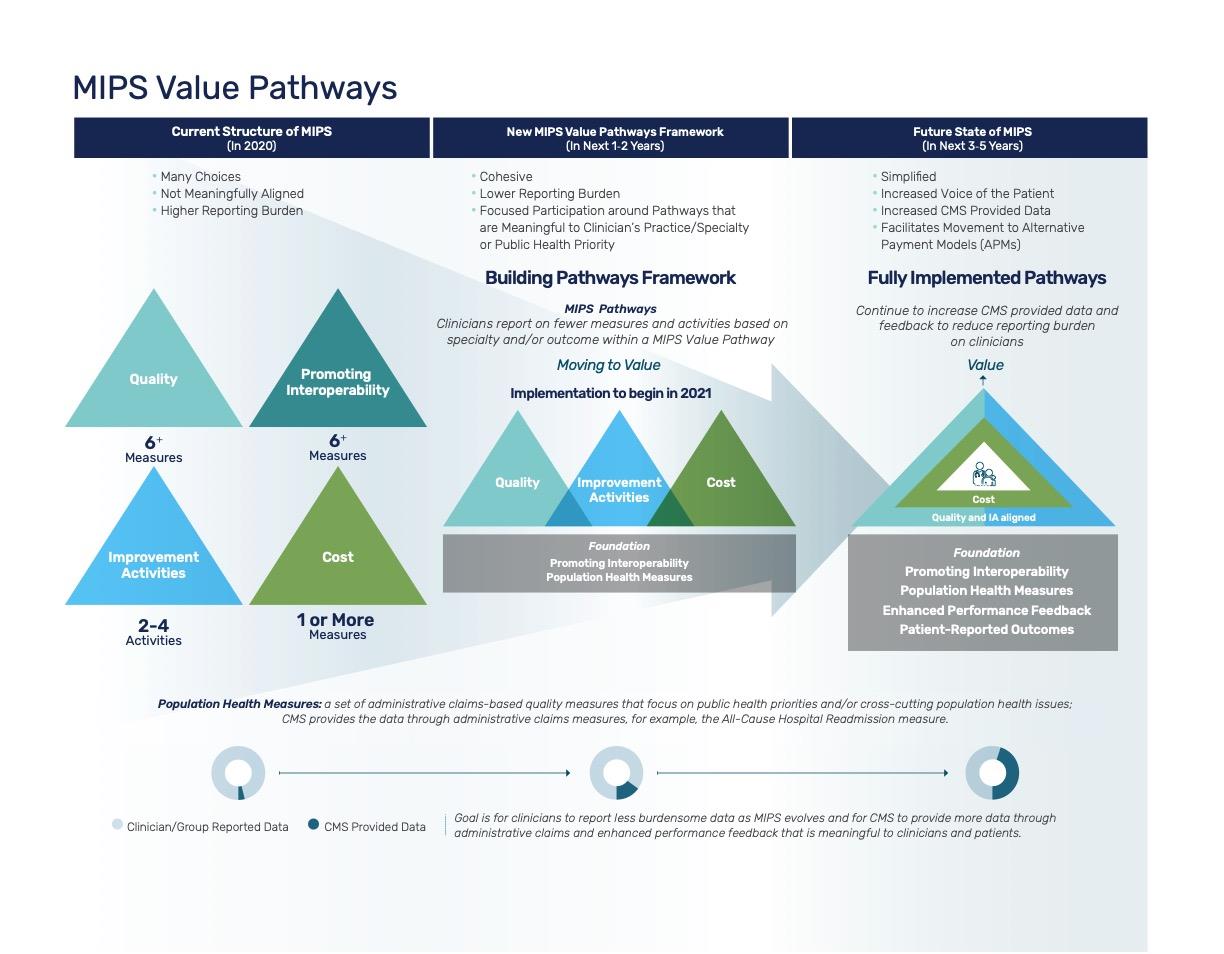
The CMS MVPs diagram shows the Quality, Cost & Improvements performance categories gradually merging into an “aligned” nutshell with a presumably-happy provider/patient pair inside, sitting on a “Foundation” which includes the Interoperability performance category and to which other non-MACRA performance categories such as “Population Health Measures” and “Patient-Reported Outcomes” will be added. Perhaps we’ll see the current non-MACRA “Complex Patients Bonus” as part of the Foundation – let’s wait and see.
We really know very little about MVPs so far, except that:
- MVPs may eventually force all providers of the same specialty to report the same MIPS Quality and Cost measures and perform the same Improvement Activities;
- CMS has been scrambling to introduce additional “specialty measure sets” for MIPS Quality and to add “episodic cost measures” so as to do justice for some threshold number of specialties;
- MVPs will be optional for 2021 and will be phased in over a number of years, to be in full effect by 2025;
- We will know more by November, 2020 by with the CMS Final Rule for 2021, and we will know more year after year as CMS makes up more rules.
Why is CMS doing this?
Of course it sounds good to simplify the MIPS program and to apply uniform performance measures within a medical specialty! For one thing, this allows more meaningful provider-versus-provider comparisons! But the MIPS framework of 4 performance categories (Quality, Cost, Improvement & Interoperability) is set in stone by MACRA and it would literally take an Act of Congress to change that! MVPs are simply way to repackage MIPS, much like a car manufacturer updating the sheet metal for the new model year but with the same drivetrain underneath; each MIPS Value Pathway must necessarily map to a combination of the original MIPS performance categories and their associated measures and activities.
Surely the “real” reason for MVPs is to drive down the MIPS median Final Scores from their 2018 levels of 99.63 out of 100.00. Any MIPS Quality measure with such a high nationwide median would be classified as “topped out” and would be removed for the next MIPS performance year! Of course, the MIPS Final Score is an essential, central concept of MIPS and cannot simply be removed. Instead, CMS recognizes that MIPS scoring is “topped out” and has an action plan to fix that: targeted rule changes with a nice name (“MVPs”) and a positive spin. Clever!
CMS has done this before: “simplifying” MIPS Interoperability for the 2019 and later MIPS performance years: by removing any flexibility regarding measure selection and thus also driving down scores. Now, participants must earn a perfect score on each remaining Interoperability measure to receive a perfect overall score! Between phasing in the Cost performance category and “simplifying” Interoperability, CMS estimated that the median MIPS Final Score for 2019 would drop by nearly 21 points from its 2018 “topped out” levels! CMS statisticians were undoubtedly pleased, or at least hopeful! In actuality, most likely CMS will not have realized its goals of dropping the 2019 median MIPS Final Score by nearly this much. We should know the final statistics for 2019 nationwide MIPS performance soon enough.
CMS appears to be repeating the same trick with MVPs: distracting us by saying: “We’ve been listening to you! You said the program was too complicated and we’ll simplify it for you!” while eliminating any flexibility in Quality or Cost measure or Improvement Activities selection! MIPS eligible clinicians may be pre-assigned their Quality & Cost measures as well as Improvement Activities, according to their medical specialty, with no flexibility to choose other measures or activities. CMS has already estimated this will serve to bring down the 2022 MIPS median score to 74.01 out of 100.00, and most likely further by 2025 once MVPs have been fully phased in.
Driving down the median MIPS Final Score is not actually a bad thing! The MIPS program was, after all, intended by Congress to be competitive, with the “average” provider earning a neutral payment adjustment, low performers receiving negative payment adjustments, and above-average or exceptional providers receiving increasingly positive payment adjustments. For this program to work as intended, in a largely budget-neutral manner and with significant financial impact on providers, the median MIPS Final Score should be reasonably distributed with its median well below 80% and ideally closer to 50%.
So we shouldn’t complain about CMS making the MIPS scoring harder with MVPs; instead, we should understand the purpose of MIPS, realize that a near-perfect 2018 MIPS Final Score is no guarantee of future MIPS “exceptional performance” and also see through CMS positive spin regarding planned program changes. If the government tells you it’s gonna be great, brace yourselves – you’re in for a ride!
Problems merging Improvement Activities into MVPs
Most current MIPS Improvement Activities are not specialty-specific, instead being “cross-cutting” in nature across a wide range of medical specialties. For example, some IAs are foundational for a practice’s quality improvement program (for example to use a structured quality improvement methodology and to require practice leadership engagement for quality improvement) while others targe care coordination or patient engagement workflow improvements applicable to any specialty. Readers might reflect on the MIPS Improvement Activities they are actively performing this year; chances are, those are cross-cutting in nature and not specialty-specific.
The MVP example for ophthalmology provided by CMS during its 2019 rule-making included the Improvement Activity “Comprehensive Eye Exams”, as the government’s best shot at reinforcing its concept of specialty-specific Improvement Activities. It’s worth going into this in detail, to illustrate a broader point. This Improvement is not actually about providing better comprehensive eye exams! Instead, it is in the “Achieving Health Equity” category and its description of reads as follows:
“In order to receive credit for this activity, MIPS eligible clinicians must promote the importance of a comprehensive eye exam, which may be accomplished by providing literature and/or facilitating a conversation about this topic using resources such as the “Think About Your Eyes” campaign and/or referring patients to resources providing no-cost eye exams, such as:
-
- the American Academy of Ophthalmology’s EyeCare America and
- the American Optometric Association’s VISION USA.
This activity is intended for:
(1) non- ophthalmologists/optometrists who refer patients to an ophthalmologist/optometrist;
(2) ophthalmologists/optometrists caring for underserved patients at no cost; or
(3) any clinician providing literature and/or resources on this topic.
This activity must be targeted at underserved and/or high- risk populations that would benefit from engagement regarding their eye health with the aim of improving their access to comprehensive eye exams.”
In simplified terms, this Improvement Activity is actually intended for family, general, or pediatric practices who should be educating Medicaid or other high-risk patients regarding the importance of comprehensive eye exams and then referring them for free eye exams! It also applies to eye care providers providing such free eye exams. It would perhaps be less confusing if CMS were to rename this Improvement Activity, for example as “Improving Access to Comprehensive Eye Exams for Underserved and High-Risk Populations”.
To make “Comprehensive Eye Exams” mandatory for all eye care providers (as was implicit in the 2019 CMS MVPs example) would force them to choose between providing no-cost eye exams or reducing their MIPS scores! It may be that the CMS staff who developed this example in 2019 did not actually understand this particular Improvement Activity or the consequences of making it mandatory for all eye care providers; in 2020, CMS dropped the ophthalmology example and switched to general surgery example instead….
That 2020 CMS specialty MVP example for general surgery specifies that surgeons must actively participate in either “Use of Patient Safety Tools” plus “Implementing the Use of Specialist Reports Back to Referring Clinician or Group to Close Referral Loop” or the higher-weighted “Completion of an Accredited Safety or Quality Improvement Program”. It may be that for many surgeons, other Improvement Activities may be better choices but the General Surgery MVP would limit their choice and may result in frustrating compliance “busy work” for many.
It is the author’s personal opinion that it would be better if CMS would not include Improvement Activities in MVPs and instead consider them to be part of the “Foundation” along with Interoperability; the author believes that CMS could reasonably achieve its goals related to MVPs by focusing only on the Quality and Cost performance categories.
Problems with CMS MIPS medical specialty categorization
The taxonomy of medical specialties is complex, as evidenced by the 200-page long AMA document on this topic. Complications include that medical specialties cannot be arranged strictly hierarchically, that there is overlap between specialties and that there are many sub-specialties to consider. CMS has traditionally over-simplified the categorization of medical specialties and has not been entirely consistent – for example the list of MIPS Quality specialty measure sets does not match the CMS Medicare provider specialty categorization perfectly.
In the past, Medicare providers may not have cared very much about the medical specialty classification CMS assigned them to, but with MVPs it will determine which MIPS measures you will be scored on and will thus affect your Medicare reimbursements! With MVPs, the clumsy CMS foray into medical specialty taxonomy will affect your bottom line!
Two general issues with CMS medical specialty taxonomy stand out:
1. Lack of acknowledgement of important sub-specialties. For example, a retina practice would clearly be left at a disadvantage with the CMS specialty measure set for general ophthalmology, since many of the measures would be non-applicable (e.g. those for glaucoma or cataracts). Does the government intend to force sub-specialists to give up their independent practices and join a broader specialty practice? Perhaps sub-specialty societies should play a more active role to raise government awareness and lobby for sub-specialty measure sets.
2. Lack of support for some Specialties. For example, despite some important overlap, optometry and ophthalmology are not the same – and there is no optometry specialty measure set! It is not necessarily clear that CMS will understand this and there is the risk that it will force the ophthalmology specialty measure set on optometry-only practices. Perhaps these so-far-uninvolved specialty societies should play a more active role to develop supplemental quality measures and lobby for their own specialty measure sets.
The good news is that we will most likely have several years in which MVPs will remain optional and the CMS problems related to medical specialty taxonomy may perhaps have been partially resolved by then.
Imagining an MVPs approach based on “most applicable measures”
Disclaimer: the following ideas are speculative and may only represent “wishful thinking” on the part of the author.
Imagine that CMS would not automatically credit a provider for the highest-scoring 6 Quality measures of whichever measures were reported by the provider or group, as is currently the case. Imagine instead an automatic “most applicable measures” selection process, for example using one of the following approaches:
- Highest volume. Quality measures could be automatically selected if the number of denominator instances (patients or visits) during the performance period place the measure in the top 6 for that provider or group; or
- Highest dollar amount. Quality measures could be automatically selected if the the Medicare fees for those denominator instances place the measure in the top 6 for that provider or group.
By way of an example with the latter model, if a provider’s total annual Medicare fees for cataract procedures are relatively higher than other types of fees, the surgeon or group would be scored on cataract outcomes, otherwise not; if a high-volume cataract surgeon would score poorly on cataract procedures, that surgeon would no longer receive top scores for Quality based on other, less-applicable measures.
For this approach to work, it makes sense that providers would need to be required to report on all possibly applicable measures – in other words those defined in their specialty measure set. Since many current MIPS Quality measures lack CMS benchmark or have benchmark problems leading to 3-point or 7-point scoring caps they should be deemed ineligible for any such “most applicable measures” scoring approach, or at least be relegated to a second tier in case no more properly-benchmarked “10-point measures” were available.
Also for this approach to be truly usable for practices, CEHRT and QCDRs should need to be certified / qualified to be “complete” relative to medical specialties, in the sense of being able to capture, calculate and report all fully eligible measures in the applicable specialty measure set(s). It would be essential that the CEHRT / QCDR combination be able to process all scorable and applicable measures for the provider, so that CMS could select the most applicable from amongst those. Only CEHRT and QCDRs certified / qualified as fully supporting the medical specialty could then be used for MIPS Quality reporting. The burden of change should shift from the provider to the HIT vendors to ensure that their systems are able to properly support the provider’s medical specialty.
Cost measure scoring already functions according to measure applicability: Cost measures are scored only if applicable, typically as soon as the denominator counts reaches 20 instances. Due to the extreme dearth of Cost measures, this approach makes sense.
Similarly, Interoperability measure scoring also already functions according to measure applicability: Interoperability measures are “excluded” under conditions of low applicability such as, for example, fewer than 100 referral orders within the performance period allowing exclusion of the “Sending Health Information” measure.
Summary: while we wait for MVPs
Succeeding with MVPs will simply translate to succeeding with MIPS measures as before, but you will lose control of the measure selection process. Do not expect your near-perfect MIPS Final Scores to automatically continue in future years. If your recent near-median performance level continues, expect to get a near-neutral future MIPS payment adjustment. If you want to earn substantial positive MIPS payment adjustments, plan to adopt a systematic, structured Quality Improvement Program for your practice, with an initial focus on monitoring and improving on your “applicable” Quality, Cost and Interoperability measures, in combination with patient satisfaction surveys. Target “exceptional performance” rather than average performance! Since most small practices lack the economy-of-scale to fully staff an effective Quality Improvement Program, consider reaching out to HiQ for a one-time free MIPS consultation, to see if HiQ should perhaps assist your practice with MVPs, MIPS and Value-Based Care in general.
HiQ will offer a public, informational webinar on MVPs after this year’s CMS Final Rule is released, with as much detail as we will know for the optional 2021 MVPs rules; this webinar is tentatively planned for December, 2020 – please check our website later in the year for registration details.
Recent Posts
- 2021 MIPS Final Rule – Practical Information and Strategic Issues December 7, 2020
- HiQ Adds Platinum Tier to MIPS EssentialsTM Service September 21, 2020
- 2021 MIPS Proposed Rule August 7, 2020
- Waiting for MVPs June 25, 2020
- Webinar – Interoperability and the Practice – June 24, July 8, & Aug 5,2020 May 11, 2020
