Checklist for 2020 MIPS
Posted on January 13, 2020
CMS has published extensive documentation on the changes to the Quality Payment Program and its MIPS track for the 2020 performance year (see references) and numerous industry reporters and pundits have already mirrored this information; the purpose of this short document is simply to provide a concise checklist of annual changes along with some recommendations for high-priority actionable items.
2020 Performance Category Weighting
| Performance Category | Standard | No Cost Score | EHR Hardship Exclusion (small practices only) | No Cost Score + EHR Hardship Exclusion |
| Quality | 45% | 55% | 70% | 85% |
| Cost | 15% | 0% | 15% | 0% |
| Promoting Interoperability | 25% | 30% | 0% | 0% |
| Improvement Activities | 15% | 15% | 15% | 15% |
Checklist of Annual MIPS Changes
-
- Thresholds and Median Scores
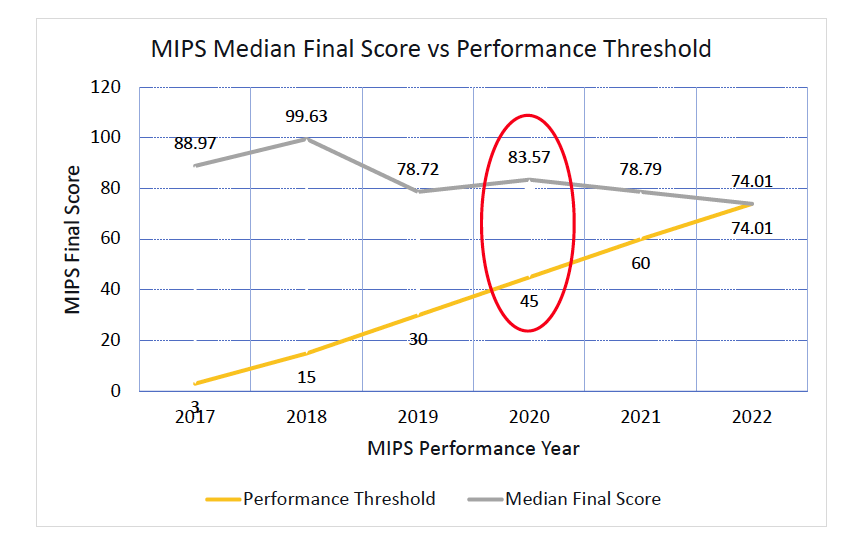
- Performance Threshold increased from 30 to 45
this is the minimum Final Score to avoid a negative payment adjustment
- Additional Performance Threshold increased from 75 to 85
this is the minimum Final Score to begin to earn higher payment adjustments for exceptional performance
- Median Score will increase from a CMS-estimated 78.72 to 83.57
this is the score of the average MIPS program participant; the expected 2020 increase will be a “recovery” from the decrease in median scores engineered by CMS via the 2019 redefinition of MIPS PI measures and scoring
- Performance Threshold increased from 30 to 45
- Thresholds and Median Scores
-
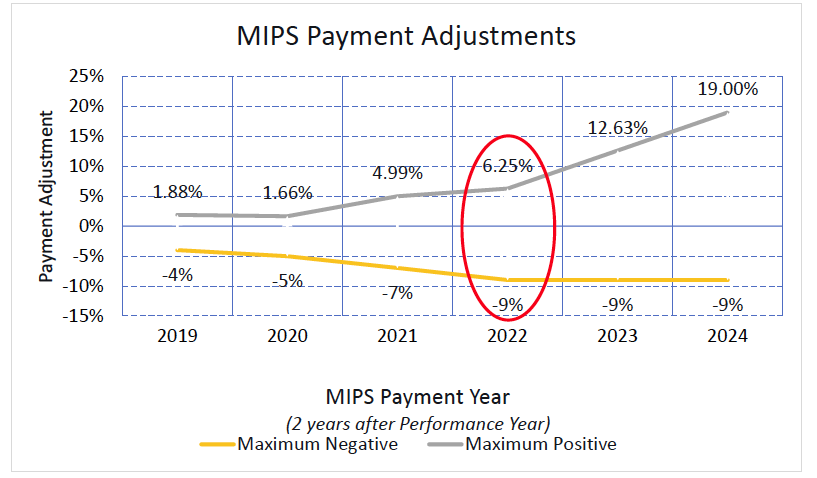
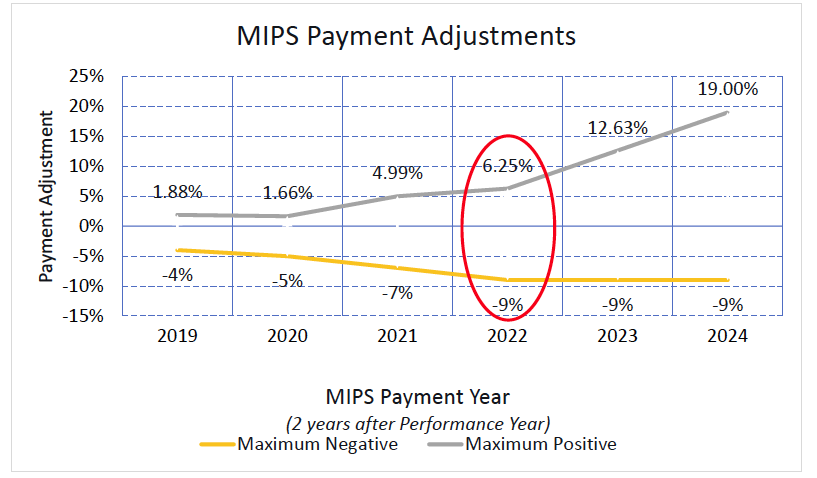
- Payment Adjustments (for the 2022 payment year)
- Maximum negative payment adjustment will increase from -7% to -9%
- Maximum positive payment adjustment will increase from a CMS-estimated +4.99% to a CMS-estimated +6.25%
- Payment Adjustments (for the 2022 payment year)
- Quality
- Data completeness threshold increased from 60% to 70%
- Removed 42 measures and added 6 specialty measure sets
- Cost
- Revised the Medicare Spending Per Beneficiary (MSPB) and Total Per Capita Costs (TPCC) measures – hopefully to reduce the amount of inappropriate attribution of these measures to specialty practices
- Added 10 episodic cost measures
- Improvement Activities
- Increased group participation requirements from 1 MIPS eligible clinician to 50% of MIPS eligible clinicians in the group
- Added 2, removed 15 and modified 7 Improvement Activities
- Promoting Interoperability
- Allowed the “unable to implement … in 2019” measure exclusion for “Receiving and Incorporating Health Information” to expire, making it more difficult to exclude from this measure
- Redefined “Query PDMP” as a non-numeric, “Yes/No” measure (retroactively for 2019 as well); this measure remains optional but eligible for bonus points
- Retired the measure “Opioid Treatment Agreement” before it ever became mandatory: apparently CMS was just kidding…
Actionable High-Priority Items
HiQ recommendations for the practice (cross-references to the list above):
- Review the MIPS Quality measures reported by the practice for 2019 to verify none have been removed; review the 2020 specialty measure sets; plan which MIPS Quality measures to target for 2020 reporting (3b)
- Review the new episodic cost measures for possible applicability for the practice; review the practice’s cost-of-care performance for any applicable MIPS Cost measures for 2020 (4b)
- Expand the practice’s Improvement Activities team to include 50% of group MIPS eligible clinicians; ensure the IAs initiative has a physician and/or executive champion (5a)
- Review practice success using Direct messaging for inbound referrals, otherwise may risk forfeiting their MIPS PI score due to mandatory “Receiving and Incorporating Health Information” measure (6a)
- If prescribing opioids and eligible for PDMP, sign up and begin to query PDMP to claim the MIPS PI bonus points (the eRx software does not need to be enhanced to provide a certified MIPS PI measure report for this purpose) (6b)
Conclusion
The transition from 2019 to 2020 MIPS will be as close to a “carbon copy” of the year before as we’re likely to see for years to come; expect CMS to significantly modify MIPS with MVPs starting in 2021 and for the program to become harder and harder…
References
- 2020 Quality Payment Program Final Rule
- 2020 Quality Payment Program Final Rule Overview Fact Sheet
- 2020 Quality Payment Program Final Rule Executive Summary
- 2020 Quality Payment Program Final Rule FAQs, Updated 11/7/2019
https://qpp-cm-prod-content.s3.amazonaws.com/uploads/739/2020%20QPP%20Final%20Rule%20FAQs.pdf
Recent Posts
- 2021 MIPS Final Rule – Practical Information and Strategic Issues December 7, 2020
- HiQ Adds Platinum Tier to MIPS EssentialsTM Service September 21, 2020
- 2021 MIPS Proposed Rule August 7, 2020
- Waiting for MVPs June 25, 2020
- Webinar – Interoperability and the Practice – June 24, July 8, & Aug 5,2020 May 11, 2020
