Improvement Activities Must Be Documented
Posted on January 6, 2020
Improvement Activities (IAs) are perhaps the most misunderstood MIPS performance category. IAs are not measures (notice that word “Activities”) and they are not a state of being (notice that word “Improvement”); they require active participation by MIPS eligible clinicians (going up from 1 per group in 2019 to 50% of the group’s MIPS eligible clinicians for 2020); perhaps most critically they require documentation which is not submitted each year but which is subject to audits.
All too often, practices allow their QCDR or QR registry to submit MIPS IAs on their behalf without so much as having any documentation of active participation by the requisite number of MIPS eligible clinicians, or sometimes without any clear understanding of what the registry submitted on their behalf. This puts the practice at risk in case of a MIPS pre-payment or post-payment audit.
Practice Responsibilities
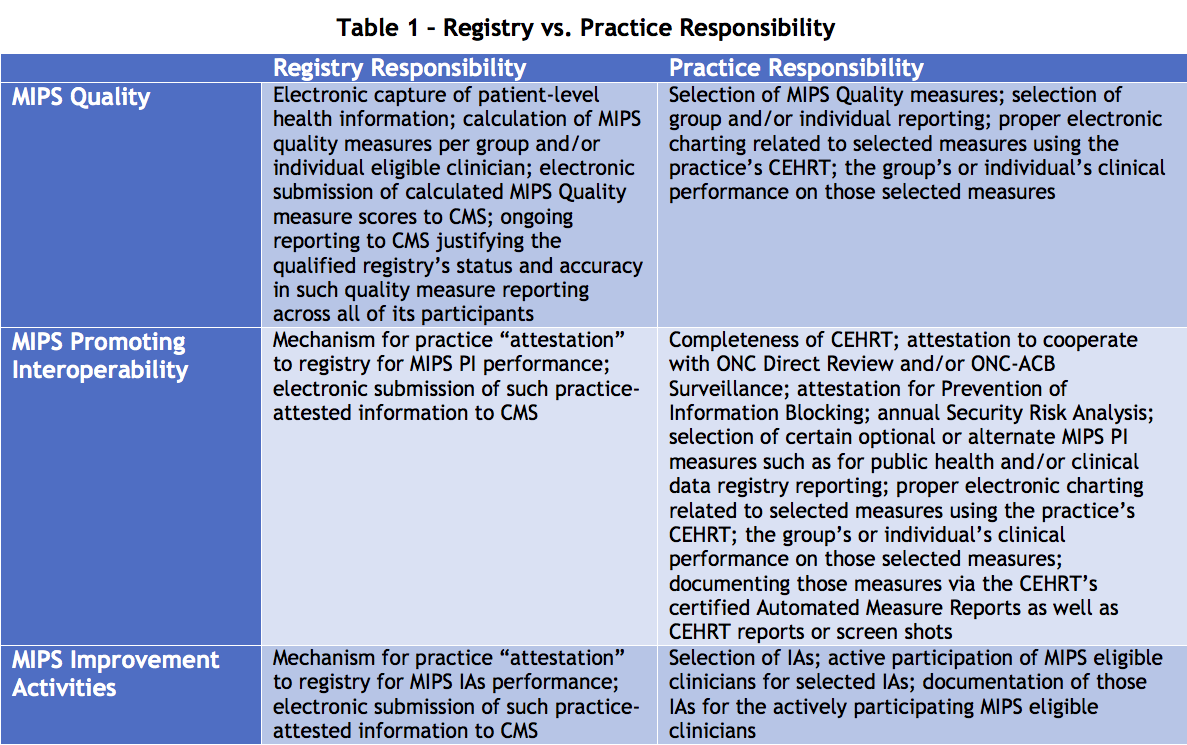
It is common and reasonable for registries (QCDRs or QRs) to not only electronically capture, calculate and submit MIPS Quality measure data for the practice but to also electronically submit MIPS IAs and PI performance data. The registry’s versus the practice’s responsibility for these MIPS submissions very much depends on the performance category:
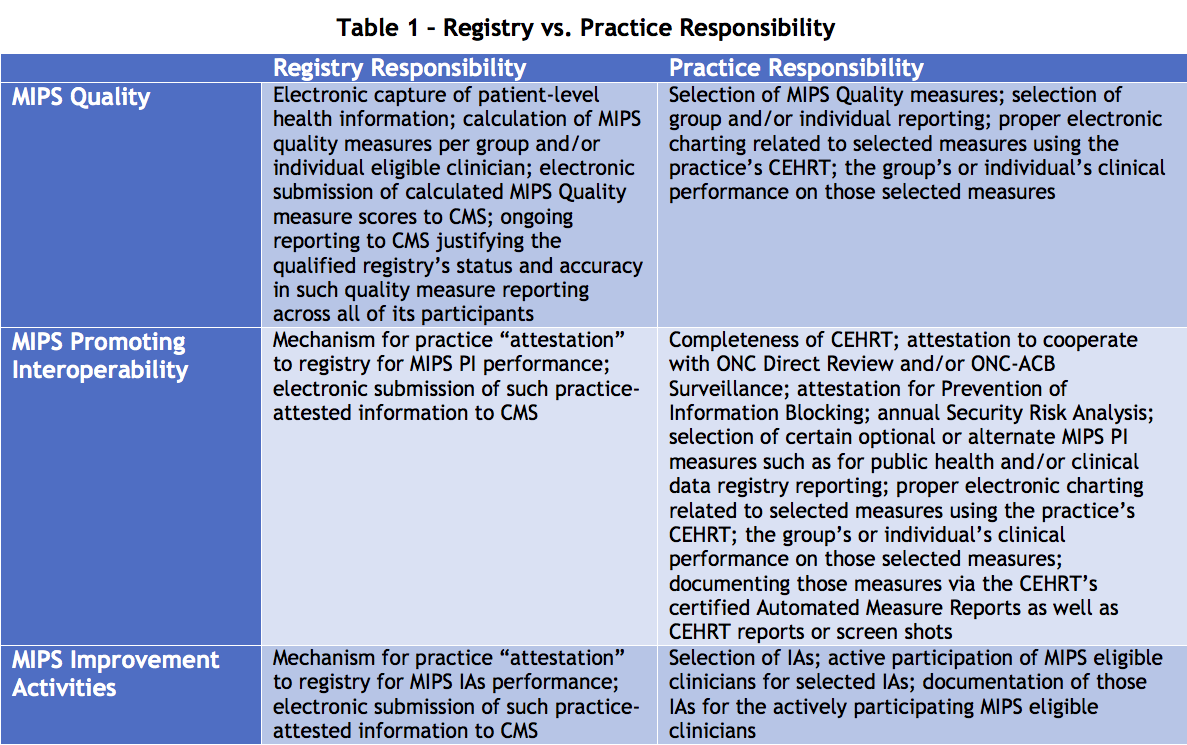
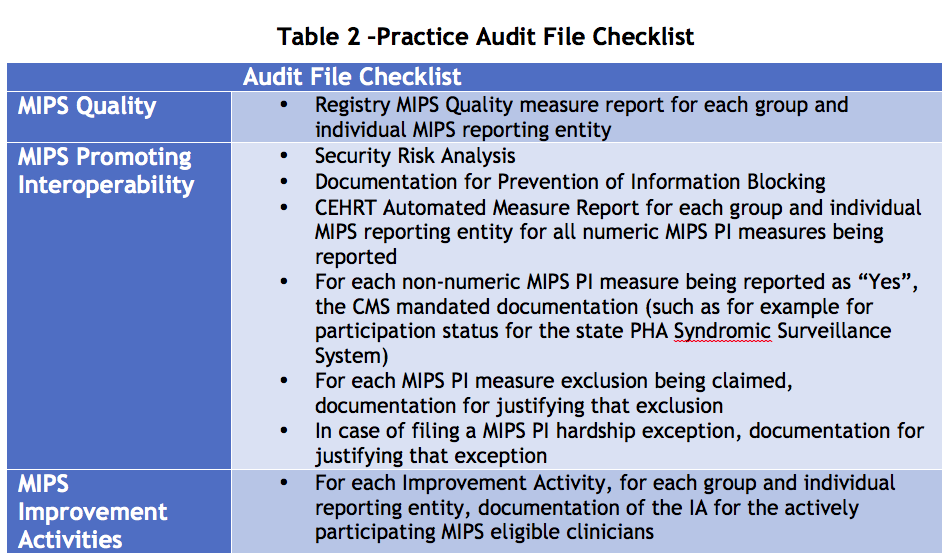
The practice must be clear that the registry has a far greater responsibility for MIPS Quality than it does for other performance categories, that for MIPS PI the practice can rely heavily on its CEHRT vendor, but that for Improvement Activities it is essentially on its own. In any case, even for MIPS Quality or MIPS PI, the practice should maintain a MIPS audit file to include at minimum the following information for each performance category
What CMS Says about Documenting Improvement Activities
Sadly, CMS requirements for documenting Improvement Activities are buried in the middle of their 2019 “Fact Sheet” (with no 2020 “Fact Sheet” yet available) and may not be immediately apparent to hapless practices. However, CMS is clear enough:
“While you do not have to submit any data when you attest to completing an improvement activity,you must keep documentation of the efforts you or your MIPS group undertook to meet the improvement activity for six years subsequent to submission. Documentation guidance for each activity can be found in the 2019 MIPS Data Validation Criteria. We suggest reviewing this validation document as you select your improvement activities for the MIPS year to ensure you document your work appropriately.”
“If a MIPS eligible clinician, group, or virtual group is selected for audit, they would be required to comply with data sharing requests, providing all data as requested including primary source documentation. CMS may reopen and revise a MIPS payment adjustment as a result of the data validation or auditing process. CMS requires all MIPS eligible clinicians, groups, and virtual groups that submit data and information to CMS for purposes of MIPS to certify to the best of their knowledge that the data submitted to CMS is true, accurate, and complete.”
The CMS “MIPS Data Validation Criteria” for Improvement Activities are in the form of a spreadsheet, with one row per Improvement Activity and with a column for “Suggested Documentation (inclusive of dates during the selected continuous 90-day or year-long reporting period)”. As an example, for the popular Improvement Activity IA_EPA_1 “Provide 24/7 Access to MIPS Eligible Clinicians or Groups Who Have Real-Time Access to Patient’s Medical Record”, the CMS “suggested” 2019 documentation is as follows:
“1) Patient Record from EHR – A patient record from an EHR with date and timestamp indicating services provided outside of normal business hours for that clinician (a certified EHR may be used for documentation purposes, but is not required unless attesting for the Promoting Interoperability [formerly ACI] bonus); or
2) Patient Encounter/Medical Record/Claim – Patient encounter/medical record claims indicating patient was seen or services provided outside of normal business hours for that clinician including use of alternative visits; or >
3) Same or Next Day Patient Encounter/Medical Record/Claim – Patient encounter/medical record claims indicating patient was seen same-day or next-day to a consistent clinician for urgent or transitional care”
Clearly, the MIPS audit file must contain this minimum level of documentation if claiming this Improvement Activity for a group or individual; in the case of a group, for 2020, the documentation must establish the active participation by 50% of the group’s MIPS eligible clinicians, so at minimum one medical record or claim per clinician.
HiQ Recommendations: Better Safe than Sorry
The practice may want to go beyond this minimum level of documentation in order to clearly demonstrate compliance with the Improvement Activity’s actual specifications, since the CMS above-quoted documentation guidelines are not subject to the annual rule making process (Proposed Rule / public comments / Final Rule) and are thus, like many other details of the MIPS program subject to CMS change without notice! For the above example Improvement Activity (IA_EPA_1), the 2019 Improvement Activity specification is as follows:
“Provide 24/7 access to MIPS eligible clinicians, groups, or care teams for advice about urgent and emergent care (e.g., MIPS eligible clinician and care team access to medical record, cross-coverage with access to medical record, or protocol-driven nurse line with access to medical record) that could include one or more of the following:
- Expanded hours in evenings and weekends with access to the patient medical record (e.g., coordinate with small practices to provide alternate hour office visits and urgent care);
- Use of alternatives to increase access to care team by MIPS eligible clinicians and groups, such as e-visits, phone visits, group visits, home visits and alternate locations (e.g., senior centers and assisted living centers); and/or
- Provision of same-day or next-day access to a consistent MIPS eligible clinician, group or care team when needed for urgent care or transition management.”
There are several general issues to point out about this particular Improvement Activity:
- The “24/7 access” is patient’s access to care, not primarily the provider’s access to CEHRT (although the patient’s access to care only counts if the provider in turn has access to the patient’s medical record);
- CMS immediately reduces the requirement of patient “24/7” access to “Expanded hours in evenings and weekends” or “use of alternatives … such as senior centers or assisted living centers…” or “same-day or next-day access for urgent care or transition management”
- One might ask, for example: expanded hours relative to what? It is not at all clear that if the practice had maintained hours of 9AM till 5PM Mondays through Thursdays but until 6PM Fridays for the last 10 days that this should count as an Improvement Activity; CMS guidelines are not clear, and it would appear to be at the discretion of the auditor; it would be far safer to document an actual process change such as introducing Saturday morning hours, or simply to select a different Improvement Activity since there are so many to choose from.
For the above example, it may be advisable to document the following additional items for each actively participating clinician:
- If claiming “expanded hours”, documentation of “normal business hours” for the clinician, and clear documentation when the example patients were seen outside of these normal business hours;
- if claiming “alternative visits” documentation of what the standard visit format is for that clinician, and clear documentation that the example patients were seen with an alternative visit format;
- if claiming “same-day or next-day access … for urgent care or transition management”, documentation of when the example patients first requested to be seen;
- That the clinician had access to the medical record during the particular patient encounters being claimed;
- More ideally, documentation such as might be expected for a Continuous Quality Improvement program, such as:
- Quantitative measures related to expanded hours, alternative visits, and/or urgent/transition appointments for all patients seen by actively participating clinicians during the MIPS IAs performance period, ideally before and after introducing a process change;
- Analysis of effectiveness of the process changes and any recommendations whether or not to adopt them as a standard process for the practice and/or to target further improvements for that process next year
HiQ recommends to select Improvement Activities to drive quality improvements in the practice and to go beyond the minimum CMS documentation guidelines so as to fully document compliance with the Improvement Activity’s specifications and intentions. Only with this pro-active approach can the practice truly benefit from Improvement Activities as well as have a reasonable level of confidence regarding the near-certain eventual MIPS audit.
—
References
- 2019 Merit-based Incentive Payment Program, (MIPS) Improvement Activities Performance Category Fact Sheet, Updated 10/16/2019
- 2019 MIPS Data Validation – Year 3 Improvement Activities Performance Category Criteria, 9/23/2019
Recent Posts
- 2021 MIPS Final Rule – Practical Information and Strategic Issues December 7, 2020
- HiQ Adds Platinum Tier to MIPS EssentialsTM Service September 21, 2020
- 2021 MIPS Proposed Rule August 7, 2020
- Waiting for MVPs June 25, 2020
- Webinar – Interoperability and the Practice – June 24, July 8, & Aug 5,2020 May 11, 2020
