Using a CQI Framework for MIPS Improvement Activities
Posted on December 21, 2019
Continuous Quality Improvement (CGI) is a conceptual framework for driving practice improvement activities, such as are mandated for MIPS Improvement Activities. CMS really fails to provide much guidance for this part of the MIPS program, but it may be helpful to take a systematic, structured approach both to maximize the actual benefit of performing Improvement Activities as well as to minimize the risk of MIPS audits revealing that little improvement and/or little activity was actually performed.
Continuous Quality Improvement Explained
There are a number of well-written summaries of CGI:
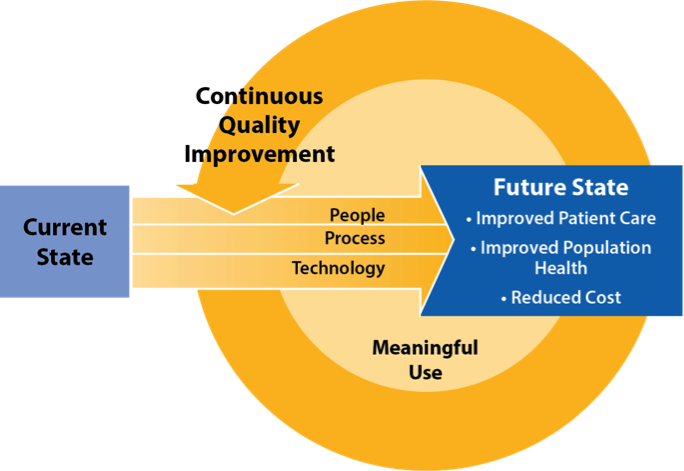
“Continuous quality improvement (CQI) is the systematic process of identifying, describing, and analyzing strengths and problems and then testing, implementing, learning from, and revising solutions. More simply, one can describe CQI as an ongoing cycle of collecting data and using it to make decisions to gradually improve program processes.” (Ref. 1)
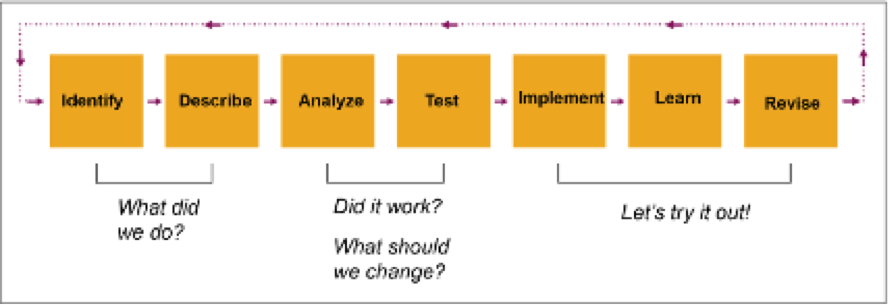
Figure 1 – The Basic CQI Process (Ref. 1)
“… CQI is a philosophy that encourages all health care team members to continuously ask: ‘How are we doing?’ and ‘Can we do it better?’ More specifically, can we do it more efficiently? Can we be more effective? Can we do it faster? Can we do it in a (timelier) way? Continuous improvement begins with the culture of improvement for the patient, the practice, and the population in general.” (Ref. 2)
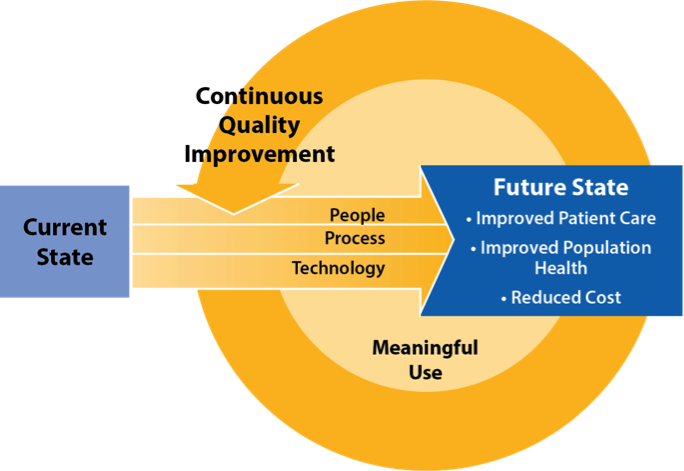
Figure 2 – Using CQI to Move From Current State to Future State (Ref. 2)
Implementing a CQI Program for MIPS Improvement Activities
Several key steps for implementing CQI to drive MIPS Improvement Activities are:
- Form an Improvement Activities Team. For an ambulatory practice organizing their MIPS Improvement Activities approach, the team may include the practice administrator, should include the resource(s) within the practice focusing on MIPS compliance, definitely should include all the MIPS eligible clinicians who will be attested as having actively participated in the Improvement Activities, should also include assistants, scribes and/or technicians to provide an alternate perspective, and may include IT, billing and other resources as appropriate.
- Identify an Executive Champion. As experience shows, any quality improvement initiative succeeds or fails depending on the support of a key decision-maker within the organization. This may typically be a physician/owner.
- Adopt a Methodology. The simple PDSA model described below may be entirely satisfactory, but other more comprehensive quality improvement methodologies (such as Six Sigma) may also be used. The author likes to keep it simple, and the PDSA model is naturally suited to the annual MIPS performance year cycles.
- Select Improvement Activities. CMS “Improvement Activities” represent topics for the CQI program; the Improvement Activities Team should select IAs which have the most potential to benefit the practice, patient outcomes and experiences and/or population health, rather than focusing on what appears to be the easiest or quickest to be done with. This typically means selecting IAs for areas in which the practice can stand to improve the most – not IAs for which the practice believes it has little or no further room for improvement.
- Select Metrics. CMS points out that IAs are not measures and that it does not define any numerators or denominators for IAs. Nevertheless, a well-organized quality improvement program will want to define metrics by which it will determine how well (or poorly) the practice is currently doing and relative to which it can evaluate the success (or failure) of process changes.
- Measure and Analyze. Selected metrics should ideally be analyzed before and after attempted process changes, to determine if these changes should become standard practice and/or whether further process changes on the same topic should be evaluated on the next MIPS performance year cycle.
PDSA Methodology
The “Model for Improvement” developed by Associates in Process Improvement, uses “Plan-Do-Study-Act” (PDSA) cycles for accelerating improvement which are a natural match for annual MIPS Improvement Activities cycles. Each MIPS performance year may represent another PDSA cycle:

Figure 3 – IHI PDSA Model (Ref. 3)
Evidence-Based Recommendations for Improvement Programs
MIPS Improvement Activities performance can benefit from prior experience with healthcare improvement programs, some of which are summarized below (Ref. 4):
“several themes emerged from successful initiatives … to guide quality improvement effort:”
- “The importance of having strong leadership commitment and support cannot be overstated. Leadership needs to empower staff, be actively involved, and continuously drive quality improvement. Without the commitment and support of senior-level leadership, even the best intended projects are at great risk of not being successful. Champions of the quality initiative and quality improvement need to be throughout the organization, but especially in leadership positions and on the team.”
- “Quality improvement teams need to have the right stakeholders involved. Efforts need to have sufficient resources, including protected staff time.”
- “Quality improvement teams and stakeholders need to understand the problem and root causes. There must be a consensus on the definition of the problem. To this end, a clearly defined and universally agreed upon metric is essential. This agreement is as crucial to the success of any improvement effort as the validity of the data itself.”
- “Efforts to change practice and improve the quality of care can have multiple purposes, including redesigning care processes to maximize efficiency and effectiveness, improving customer satisfaction, improving patient outcomes, and improving organizational climate.”
- “Appropriate use of technology can improve team functioning, foster collaboration, reduce human error, and improve patient safety.”
- “Change takes time, so it is important to stay focused and persevere.”
Conclusion
A systematic approach to a CQI program can ensure that MIPS Improvement Activities are performed without risks of MIPS audits and that substantial benefits will be achieved for the success of the practice business outcomes, for patient outcomes and experiences as well as for population health management.
HiQ recommends its clients invest in a serious effort to drive MIPS Improvement Activities, not merely a pro-forma approach of attesting without taking any new action.
References
- Continuous Quality Improvement, Office of Adolescent Health: https://www.hhs.gov/ash/oah/sites/default/files/cqi-intro.pdf
- Continuous Quality Improvement (CQI) Strategies to Optimize your Practice, provided by The National Learning Consortium (NLC), developed by Health Information Technology Research Center (HITRC), April 30, 2013: https://www.healthit.gov/sites/default/files/tools/nlc_continuousqualityimprovementprimer.pdf
- How to Improve, Institute for Healthcare Improvement: http://www.ihi.org/resources/Pages/HowtoImprove
- Patient Safety and Quality: An Evidence-Based Handbook for Nurses, Tools and Strategies for Quality Improvement and Patient Safety, Ronda G. Hughes, National Center for Biotechnology Information, U.S. National Library of Medicine: https://www.ncbi.nlm.nih.gov/books/NBK2682/
Recent Posts
- 2021 MIPS Final Rule – Practical Information and Strategic Issues December 7, 2020
- HiQ Adds Platinum Tier to MIPS EssentialsTM Service September 21, 2020
- 2021 MIPS Proposed Rule August 7, 2020
- Waiting for MVPs June 25, 2020
- Webinar – Interoperability and the Practice – June 24, July 8, & Aug 5,2020 May 11, 2020
